Pilot Study
Exercise Restraint for Early Mobilization and Sedation Minimization in Intubated Patients
MT Pavini MD, J Washburn BSN, RN, CCRN. Department of Critical Care, Rutland Regional Medical Center, VT
Disclosures: MT Pavini MD is the developer of the restraint alternative.
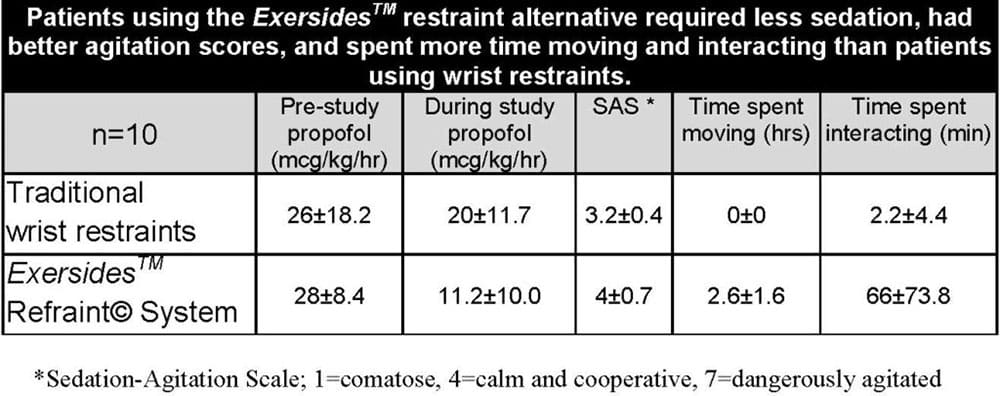
Background: Restraint usage is an important part of keeping patients safe but creates immobility. Wrist restraints severely limit mobility and patients often place head to hand for self-extubation. With mitt restraints patients can squeeze them onto the endotracheal tube (ETT) for self-extubation. We hypothesized that a restraint alternative that allows movement without access to the ETT would lead to better in-bed mobility. The restraint alternative does not require being tied to the bed and allows arm mobility and exercise. Methods: We enrolled 10 intubated patients and alternatively assigned them to wrist restraints or restraint alternatives. On day #3 of intubation, all patients were videotaped for 4 hours while wearing their assigned device. All patients had usual sedation minimization ordered by the attending physician and directed by the nurse. Patient sedation, in-bed movement and interaction with staff and family members were recorded. Evaluation Forms were completed by the Nurse, Family and Patient (if able).
Results: Patients in the restraint alternative had more in-bed movement, less sedation, better SAS score, and preferred the restraint alternative. Families and nurses preferred the restraint alternative. There were no ETT dislodgements. Conclusions: Intubated patients remained safe and were more mobile in the restraint alternative. Patients, families and nurses preferred the restraint alternative.
Exersides NIH FREEDOM trial
Phase I has been successfully completed and proved safety. Phase II has now completed enrollment at the University of Vermont Medical Center, Johns Hopkins, and the University of California San Diego. Results to be published soon. Details here.
Research reported in this publication was supported by the National Institute on Aging of the National Institutes of Health under Award Numbers R42AG059451 and SB1AG073026. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
PADIS GUIDELINES 2018
Clinical Practice Guidelines for the Prevention and Management of Pain, Agitation/Sedation, Delirium, Immobility, and Sleep Disruption in Adult Patients in the ICU Devlin, John W. PharmD FCCM (Chair)
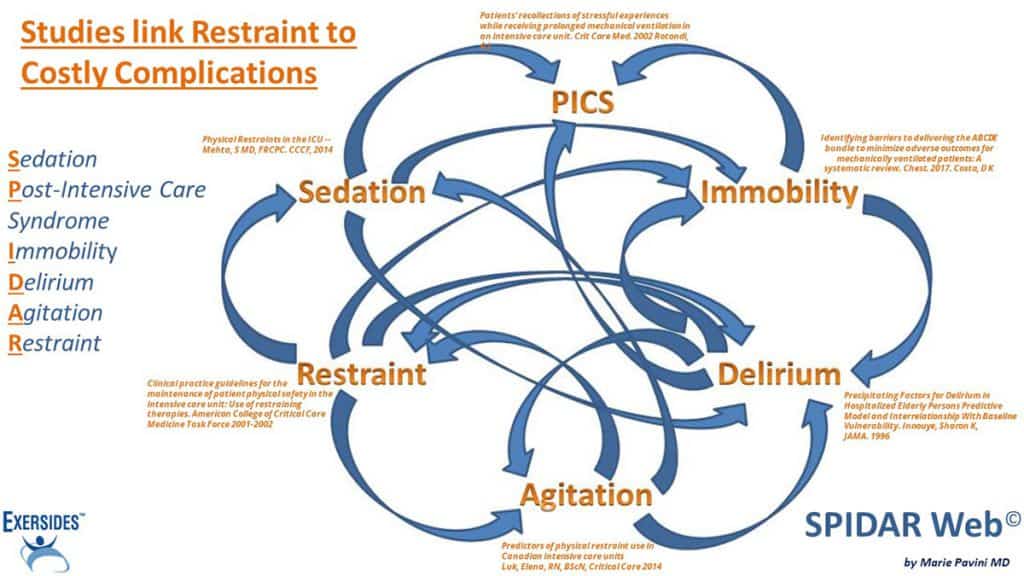
In an era focused on improving patient-centered care, the effect physical restraints have on the care and outcomes of critically ill adults remains controversial. …studies exploring physical restraint use and outcomes of the critically ill paradoxically report higher rates of the events that their use is intended to prevent. These events include more unplanned extubations and frequent reintubations; greater unintentional device removal; longer ICU LOS; increased agitation; higher benzodiazepine, opioid, and antipsychotic medication use; and increased risk for delirium or disorientation.
Patients’ perceptions of being physically restrained during an ICU stay vary but often provoke strong emotional responses that persist after the ICU stay. Given the prevalence, unintended consequences, and patients’ perceptions of physical restraint use, critical care providers should closely weigh the risks and benefits of this practice in the adult ICU setting before initiating or maintaining physical restraint use. Although certain countries report a “restraint-free” ICU environment, it may be possible that their use of bedside sitters and/or pharmacologic restraints is increased.
ACCM Clinical Practice Guidelines
Clinical practice guidelines for the maintenance of patient physical safety in the intensive care unit: Use of restraining therapies. American College of Critical Care Medicine Task Force 2001-2002 . Maccioli, Gerald A. MD, FCCM; Dorman, Todd MD, FCCM
RECOMMENDATION: The choice of restraining therapy should be the least invasive option capable of optimizing patient safety, comfort, and dignity.
Nurses and Restraints
The challenges of using physical restraint in intensive care units in Iran: A qualitative study. Salehi Z, Joolaee S, et al. J Intensive Care Society 2020 Jan.
RESULTS: Related to nurses’ distress over Physical Restraint use.., namely emotional and mental distress, moral distress, and inability to find an appropriate alternative for Physical Restraint.
Complications and Restraints
The effect of physical restraint on neurovascular complications in intensive care units. Ertugrul B, Ozden D. Australian Critical Care 2020 Jan; Vol 33, Issue 1, Pages 30–38.
RESULTS: Prolonged physical restraint led to a shortage of blood flow and pressure on nerves and tissues with consequent damage.
Incidence, risk factors and outcomes of delirium in mechanically ventilated adults. Crit Care Medicine 2015 Mar; 43(3):557-662014. Mehta S, Cook D, Devlin JW, et al, for the SLEAP Investigators and the Canadian Critical Care Trials Group.
RESULTS: Restrained patients had: Lower APACHE ll mean scores; More delirium; More device removal; More reintubation; All statistically significant
Delirium and Restraints
Precipitating Factors for Delirium in Hospitalized Elderly Persons Predictive Model and Interrelationship With Baseline Vulnerability. Innouye, Sharon K, MD, MPH; Charpentier, Peter A., MPH JAMA. 1996;275(11):852-857
RESULTS: …independent precipitating factors for delirium… : use of physical restraints (adjusted relative risk [RR], 4.4; 95% confidence interval [CI], 2.5 to 7.9)
Predictors of Physical Restraint Use
Predictors of physical restraint use in Canadian intensive care units Luk, Elena, RN, BScN, Critical Care 201418:R46;DOI:10.1186/cc13789
RESULTS: Restrained and never-restrained patients had similar baseline characteristics… however, restrained patients were agitated and over-sedated…more…
Sedation and Physical Restraints
Physical Restraints in the ICU. Mehta, S MD, FRCPC. Univ Toronto, Canada. CCCF October 30, 2014
RESULTS: Daily sedation interruption assoc with more restraint use (OR 1.84, 95% CI 1.27, 2.67)
Early Mobilization and Restraints
Early mobilization of critically ill adults: a survey of knowledge, perceptions and practices of Canadian physicians and physiotherapists
Karen K.Y. Koo, MD, MSc, Karen Choong, MB, MSc, Deborah J. Cook, MD, MSc, Margaret Herridge, MD, MPH
| Patient barrier | All clinicians (n=311) | Physicians (n=194) | Physiotherapists (n=117) |
| Physical restraints | 64 (20.6%) | 50 (25.8%) | 14 (12.0%) |
| Excessive sedation | 187 (60.1%) | 112 (57.7%) | 75 (64.1%) |
Identifying barriers to delivering the ABCDE bundle to minimize adverse outcomes for mechanically ventilated patients: A systematic review. Chest. April 27, 2017. Costa, D K, PhD, RN
RESULTS: “Perceived patient barriers to early mobilization in the intensive care unit: Patient and staff safety concerns”
PICS and Post-Traumatic Stress
Patients’ recollections of stressful experiences while receiving prolonged mechanical ventilation in an intensive care unit. Crit Care Med. 2002 Apr;30(4):746-52. Rotondi, A J
RESULTS: 44.8% remembered being restrained; 86% of those were moderately to severely bothered by it.
Psychological sequelae following ICU admission at a level 1 academic South African hospital. SAJCC. Nov 2010,Vol 26,No 2. Hatchett, RN,RM,Ned,ChN,BACur,BA,MSc
RESULTS: An unexpected finding of this study was that patients who had memory of physical restraints in the ICU were six times more likely to develop symptoms of PTS than those with no memory of physical restraints.
Use of physical restraints in adult ICU patients to prevent patient-initiated device removal: a systematic review Università di Bologna Facoltà di Medicina e Chirurgia Master in Evidence Based Practice e Metodologia della Ricerca Clinico Assistenziale
RESULTS: One third or more of the self-extubation events occurred despite use of wrist restraints leaving the effectiveness of physical restraints an unresolved issue… as it can heighten agitation and may have devastating physical and psychological effects on the patients.
In The News
NY Times (07/22/2013): Nightmares After the I.C.U.
PBS News Hour (06/16/2017): Why a stay in the ICU can leave patients worse off
WSJ (03/02/2018): How to Minimize Permanent Mental Trauma from an ICU Stay
NY Times (08/01/2018): Take a Vacation From Exercise? Your Body May Not Thank You: Two new studies look at what happens when we do not exercise or move around much for a period of time.