The most common barriers to mobilizing children are lack of physiotherapy resources, lack of practice guidelines, equipment and concerns for patient safety. Families’ trust in the healthcare team and clinicians’ belief in the importance of early mobilization were the most supportive reasons for early mobilization in the PICU population and facilitated patient motivation.
Implementation of an early mobilization activity program has shown to decrease the immobility caused by procedures or tests. However, the reported barrier of equipment availability increased.

Mobilization of critically ill children, many with central lines, endotracheal tubes, and other life-saving devices, is associated with potential risks and complications. Hence, concerns about safety often guide staff perceptions about PICU mobility. These complications may include, but are not limited to, hemodynamic instability, accidental tube or line dislodgement, falls, pain, and anxiety. However, multiple studies have reported that early mobilization of critically ill children is safe when appropriate precautions are taken, and levels of mobility are suitable for the level of acuity.
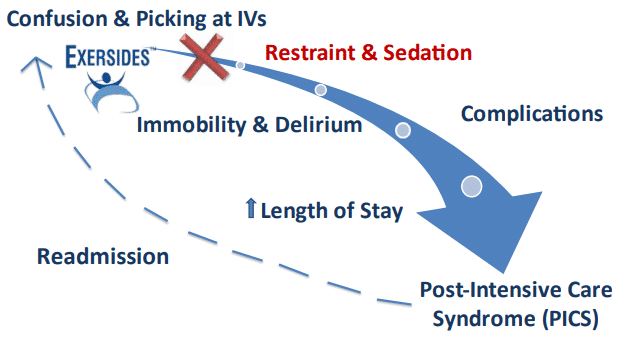
Children who were allowed a more liberal activity level postoperatively, specifically without physical or pharmacological restraints, had shorter PICU and total hospital lengths of stay to breaking down the wall of immobility culture.

Heavy sedation, bedrest, and delirium contribute to a PICU culture of immobility. Clinical benefits of mobilization have been demonstrated yet fewer than 25% of critically ill children mobilize early in the children’s PICU stay.
This finding suggests that team coordination for mobilization activities was improved and that missing specialized equipment became more apparent as mobilization was considered for patients previously deemed ineligible.
The Exersides Refraint System solves the issue of having specialized mobilization equipment.
Optimizing sedation goes hand in hand with a culture of mobilization to facilitate patient engagement. When targeting mobility, it is crucial that frequent sedation assessments and adjustments to sedation medication be made to ensure that a child is as awake as is safely feasible.
Maintaining children in an alert, lucid, and comfortable state during the daytime hours and optimizing restorative sleep at night is an essential first step to breaking down the wall of immobility culture.
